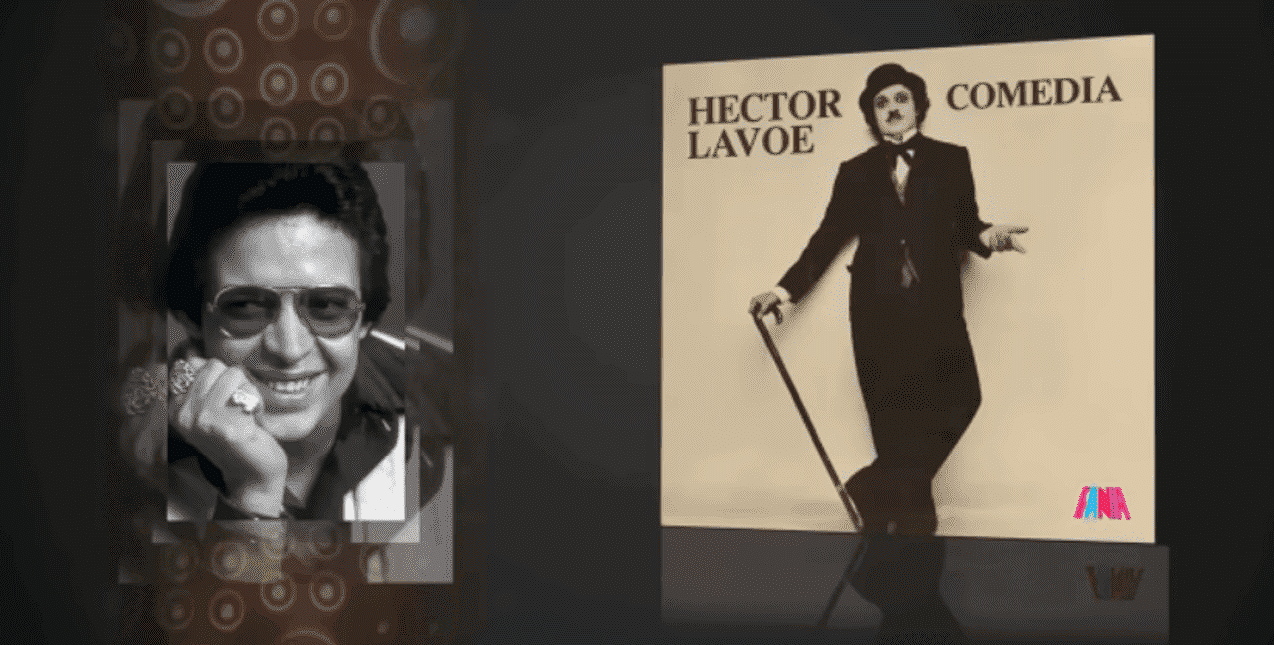
Graphic by Desiree Tapia, Photo courtesy of Xanadu Roque
The three major insulin makers announced in March that they would implement monthly price caps and/or lower the list price of insulin. The moves came after years of activism from diabetics and the passage of two federal laws that pressured the companies to act.
What’s it like to ration insulin because you can’t afford it? What’s it like to vomit water and wind up in the hospital as a result?
Gainesville resident Xanadu Roque knows all too well. Roque is a Type 1 diabetic who was diagnosed at age 12. She relies on insulin to survive and has dealt with a lot of stress and sickness over the years trying to maintain access to a steady supply of the expensive medication.
For years, the three major insulin makers steadily raised the prices of the life-saving medication—so much so that over a 20-year period, the cost of insulin increased by 600%. These price hikes came as the cost of producing insulin remained stable, between $3.69 and $6.16 a vial, according to one 2018 study.
The skyrocketing costs forced diabetics to spend several thousand dollars—and sometimes tens of thousands of dollars—a year on the medication.
But thanks to pressure from advocates like Roque and the actions of Democratic lawmakers, the tide has finally begun to turn.
Between March 1 and March 16, the three major insulin makers that make up roughly 90% of the market—Eli Lilly, Sanofi, and Novo Nordisk—announced that they would implement a $35 monthly cap for those with private insurance and/or lower the list prices of their products by between 70-78%, effective Jan. 1, 2024. Individuals without insurance will also have access to lower prices.
The announcements came after President Biden’s Inflation Reduction Act capped out-of-pocket insulin costs for seniors on Medicare at $35 per month. Biden’s American Rescue Plan also reformed the rules guiding the Medicaid health insurance program so that the companies would have faced a financial penalty had they not lowered their prices.
We recently interviewed Roque to hear her story and get her thoughts on the announcements.
This interview has been edited and condensed for brevity and clarity.
Floricua: Can you tell us about your story and what it’s been like living with diabetes?
Xanadu Roque: My story is kind of an interesting one. I was diagnosed when I was 12 years old. I have traditional Hispanic parents, so that kind of means that they didn’t really understand what diabetes was, so for my youth, I kind of had a rocky start with diabetes. I kind of took care of myself for a little bit when I was really, really young. And then after a while, as a teenager, I wanted to do what I wanted, I didn’t want to take insulin, I didn’t want to check my blood sugar.
And then when I turned 18 or 19, I didn’t have insurance anymore and I couldn’t afford insulin, couldn’t go to the doctor, didn’t know any resources, didn’t know other people with diabetes. I had insulin kind of saved up from when I had insurance, but eventually that ran out.
I was rationing my insulin for a while. I ended up in the hospital really, really sick, to the point I was vomiting water. And they were like, ‘If you didn’t come here now, you could have ended up in a coma or worse.’ After that, I found some resources and started going to a federally qualified healthcare center. That was very lifesaving for me, but it still wasn’t great because I still didn’t know what I was doing. I had a primary care physician instead of an endocrinologist. I couldn’t afford to go to an endocrinologist out-of-pocket.
When I moved from [Miami] to Gainesville, I started school here. I ended up doing a research project that introduced me to other people with diabetes, and ever since then, I’ve changed the trajectory of my life to work in diabetes just because I’ve been affected and impacted by it so much.
I know what it’s like to not be able to afford your insulin or doctors appointments, to go to a doctor and be belittled by doctors who don’t understand what you’re going through. I understand what it’s like to also then have insurance and be on an insulin pump. Now I have a continuous glucose monitoring device. Everything’s going great, but from not taking care of myself when I was younger, I also have some eye damage, which is thankfully the only thing that’s happened. It could be much worse, so I’m very thankful that everything else is fine. It’s just been a crazy rollercoaster ride of an experience.
How long were you rationing for and what was that like? Did it have a psychological toll?
I was probably rationing for five months, honestly. And at the time, I used to be a person who wasn’t very outspoken. I was very shy. I don’t like bothering people or anything, so I didn’t tell anybody in my family. Nobody knew. So by the time I ended up at the hospital, people were like, ‘What the hell happened? Why didn’t you ask for help? Why didn’t you do anything?’
I think that really taught me that people are here to help you. You shouldn’t be afraid of asking for help. And thankfully, I do have a really good support system in that sense. But I think for me, rationing insulin was just such a very to-myself type of thing. And it was really, really scary. I had a lot of anxiety. I was really stressed out because I knew my blood sugars were high. But it came to a point where I just stopped checking my blood sugars and I was like, ‘If I don’t know, it doesn’t exist.’
Obviously, that’s not how the world works, but that’s kind of just how I saw it. And then going to the hospital and them telling me everything that happened. At that time, I don’t think I understood how serious it was. It wasn’t until after the fact and learning more about how people do this and they end up passing away that I realized how serious that really was for me and how I could have really almost died. I was right there. I was vomiting water by the time I ended up in the hospital.
Did you get insurance after you got out of the hospital, or was there still a period of time after that where you were uninsured?
I was uninsured for probably two to three years after that, because I didn’t really get insurance until Obamacare happened. I looked for insurance, but it was just too expensive. It was literally maybe a hundred and something dollars every month and I was working a part-time job at Forever 21. Couldn’t really do that, so yeah, I didn’t have insurance for a while.
So were you paying the list price at that point? You said you were connected to some resources, how did that work?
I mentioned federally qualified healthcare centers, because in Florida—I think all of them have this—but they have a drug program in which insulin is $25 every time you get it. So instead of paying the out-of-pocket price, as long as you’re going to that federally qualified healthcare center, you’re able to get insulin for $25. But you have to make sure that you’re seeing your doctor at least once a year, which wasn’t always the case for me because I got busy.
Do you know what the most you’ve ever paid for a vial or a month’s supply is?
I don’t remember. It was a while ago, where my godparents ended up paying, I think, 200-and-something dollars for it, so I think that’s been the most that I paid for it, thankfully.
Are you insured through your employer right now? What are you paying for insulin now?
Yeah, [through my employer]. It’s about $90 for three months, which isn’t bad honestly, but I know of some people who obviously can’t afford that. But I’m thankful that my insurance is pretty good for now.
The three big insulin makers all announced in March that they’re either going to implement copay caps for people on private insurance or drop the list price or both. What was your reaction to those announcements?
I was happy about it. All my family and friends obviously know I have diabetes, so I was getting a lot of TikToks sent to me and Instagram messages sent to me. And I’m like, ‘Yeah, that’s great, but where was this 10 years ago,’ when not only I needed it, but how many people have had to die in order for this to happen?
I think it’s a really good step in the right direction, but also working with people who are very underserved, some people can’t even afford that, and I think that’s something that especially lawmakers don’t get. Maybe they’ve had to struggle, but I don’t think they’ve really had to struggle. I think that it is a great step in the right direction, advocacy is working, but it isn’t as great as I would have wanted it to be.
I know you’re in a good situation right now in terms of your insulin, but do you think these changes will affect people you know in the diabetes community?
I work with very marginalized people who can’t afford their insulin, who are still struggling. So could this help? Yeah. But you still have people who are on other insulins that aren’t seeing price cuts, so making insulin free would be one of the ways you could help everybody. This will affect a lot of people in the sense that it can be good for some people, but there are still going to be people falling through the cracks.
Politics

Biden administration bans noncompete clauses for workers
The Federal Trade Commission (FTC) voted on Tuesday to ban noncompete agreements—those pesky clauses that employers often force their workers to...



Video: Debbie Mucarsel-Powell: The Six-Week Abortion Ban Is An Attack on Democracy
Local News



Biden administration bans noncompete clauses for workers
The Federal Trade Commission (FTC) voted on Tuesday to ban noncompete agreements—those pesky clauses that employers often force their workers to...